Centricity Eligibility Verification
Centricity® Integrated Patient
Verification
Centricity Eligibility Verification
pVerify’s First-Class Batch Eligibility Verification Solution automates patient verification within Centricity® with no manual effort.

Integrate pVerify
to your Centricity® Software
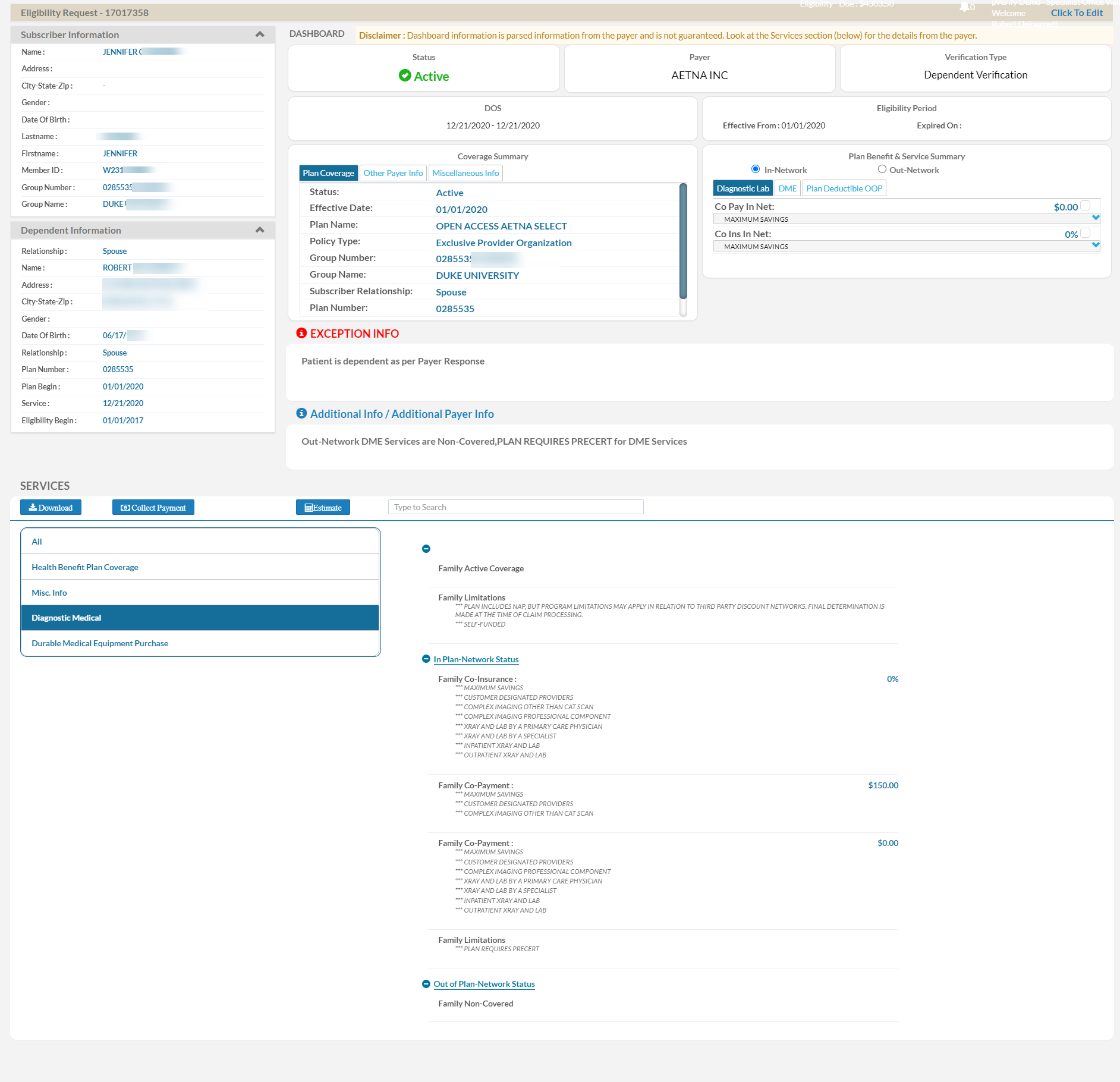
pVerify offers Centricity Eligibility Verification Integrations to outsource patient verification for full DOS or specific services. Custom specifications pull all patients for a specific date or a customized set of patients based on Provider, Appointment Type, Payer, or additional parameters. Verified days in advance, users are able to view the patient benefits in a completed Excel file and directly in the patient’s appointment notes.
Experts in patient insurance verification, pVerify is able to capture copays and co-insurance for multiple services in one verification. Additionally, they can go further by providing additional information unique to each industry, such as Routine Visit details for Ophthalmology, visits remaining out of allotted for Physical Therapy, and Surgical details based on the location of the procedure.
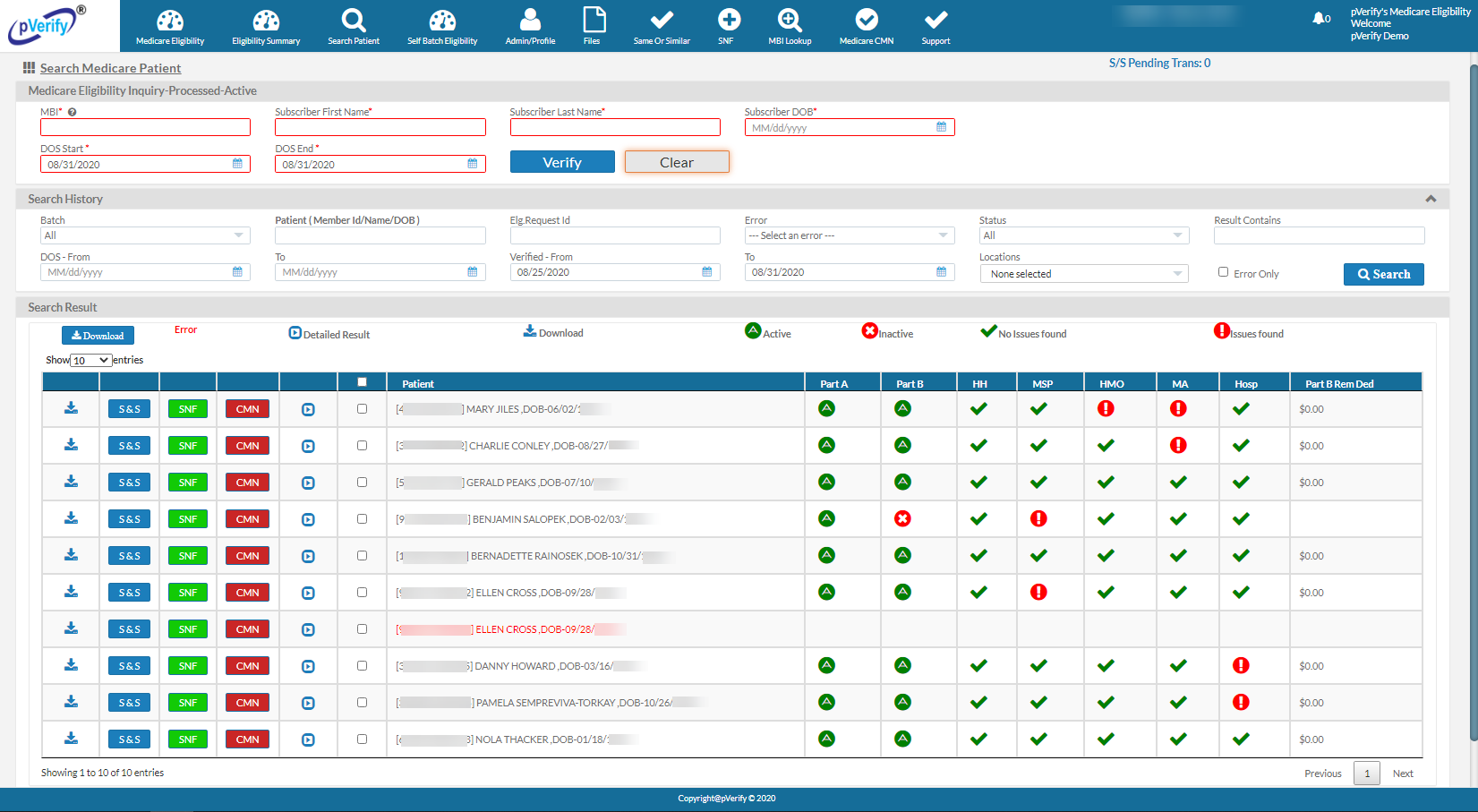
As the only company to provide traditional patient verification for EDI payers plus human-enabled AI verification of more difficult Non-EDI Payers, they have the largest payer list in the industry. Featuring Medical, Vision, and now Dental Payers, pVerify can verify every patient on your schedule.
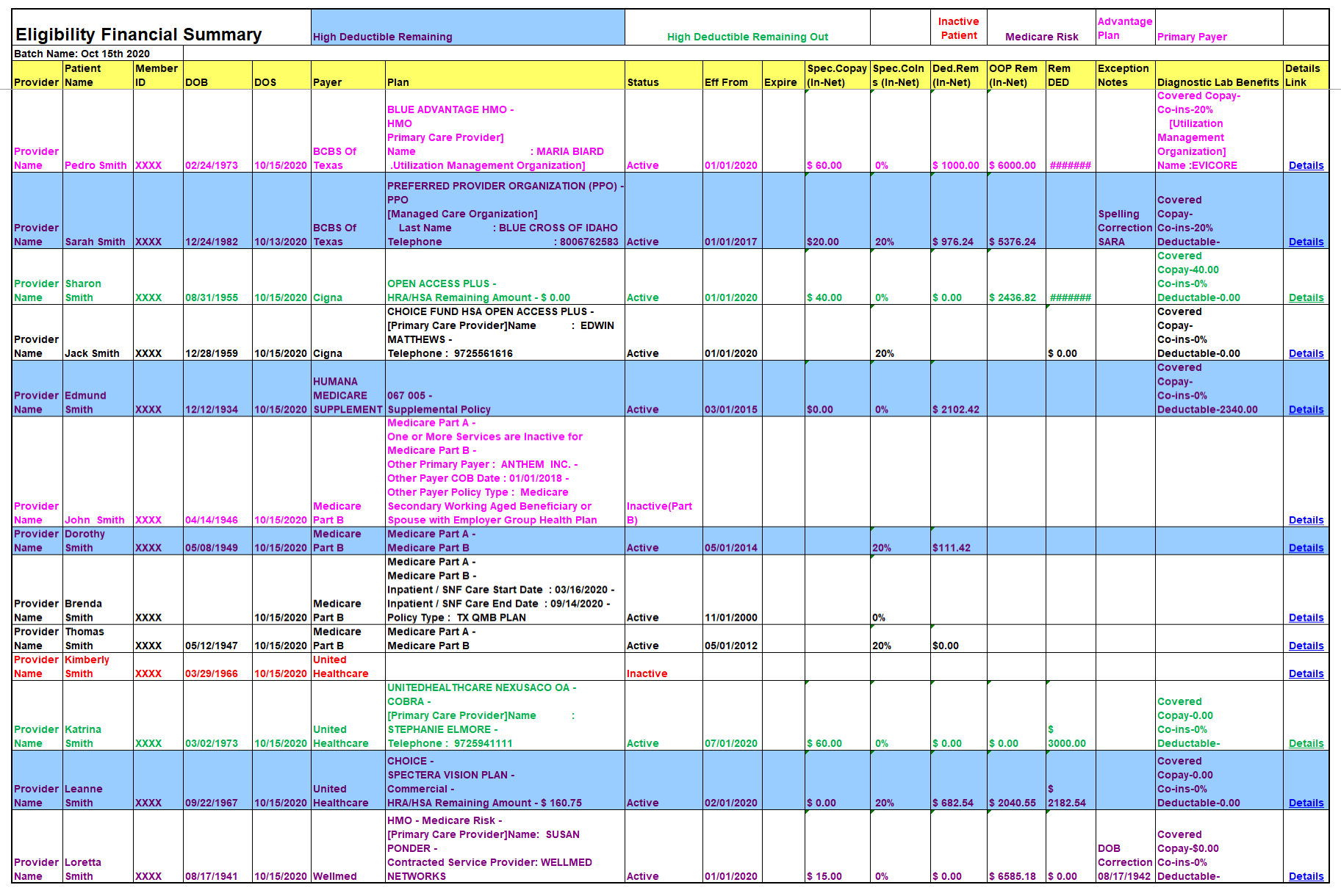
pVerify’s signature solution, First-Class Batch Reports take patient verification to the next level. pVerify provides a completed report in Excel format with all of your requested patient benefit information. Color-coded font and highlighted rows help identify and flag specific patients: High Deductible, Medicare Risk, HMO Detection, and others, per request. Each patient is linked to their full patient record, within the pVerify Premium Portal, for additional patient benefit review.
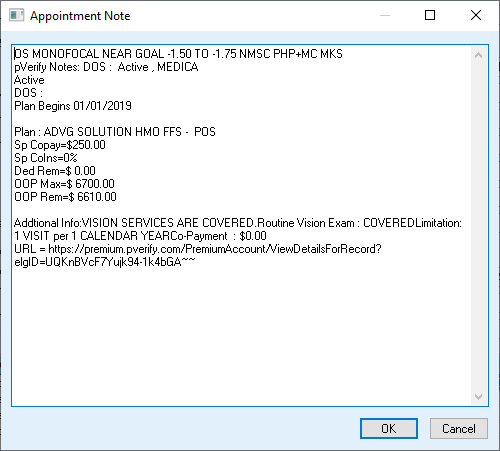
As part of the pVerify Integration, each patient’s verified benefits are inserted directly into their patient record in the form of a quicknote. This allows staff to review the patient’s benefits in their appointment schedule and on pVerify’s custom Batch Report, as well as directly in the pVerify Portal.
Learn how pVerify’s Centricity Eligibility Verification Solutions can automate your patient verification needs!
Centricity® Integrated First-Class Batch Eligibility
Verification by pVerify®
pVerify is the only company to offer a combination of EDI-based eligibility, human-enabled AI, machine learning, and manual, live operator-assisted processing to return all the relevant information complete and contextual.
Effortless and automatic, pVerify Centricity Eligibility pulls appointment data directly for a specific DOS, Provider, or Appointment Type.
Verified daily, weekly, or monthly, pVerify manages the difficult payers (Non-EDI) through human-enabled AI, machine learning, and manual effort.
The patients pulled for the DOS verification can be broken down by provider, appointment type, or service, ensuring only the patients that need to be verified will be pulled.
pVerify capture’s copays and co-insurance for multiple services in one verification plus unique details, in addition to the deductible and OOP remaining.
Unique benefits, such as Routine Visit details for Ophthalmology and Surgical details based on the location of the procedure, can be added.
The color-coded and highlighted Excel file helps identify and flag specific patients: High Deductible, Medicare Risk, HMO Detection, and others, per request.
Each patient in the Excel file is linked to their full patient record within the pVerify Premium Portal for additional patient benefit review.
pVerify inserts each patient’s verified benefits directly into their patient record in the form of a quicknote.
pVerify has the largest payer list comprised of EDI and Non-EDI Medical, Vision, and Dental Payers.
Learn more with a custom DEMO or Free Trial
Meet with a pVerify Representative to assess your current work flow and unique requests to determine the best combination of pVerify's Eligibility Solutions for your needs.
Featured Clients
pVerify works with clients in some of the largest Medical Practices, IPAs/MSOs, and Medical Billing companies. We have a very strong presence in Primary Care, Therapy (speech, occupational & physical), Orthopedics, Sleep Centers, and Imaging Centers.

Oklahoma

Texas
New York
California
California

Louisiana

Oklahoma

Maine

California

North Carolina

Texas

California

Oklahoma

California

Oklahoma

California

New Jersey
Verify – Estimate – Collect
Our automated, date-of-service patient insurance verification brings unprecedented efficiency to your front-office workflow. Coupled with our Patient Estimator and hands-free Patient Payment, our Solutions can significantly reduce patient debt and improve front-office collections.
Advanced Eligibility
Verify a patient ahead of time or during their procedure with pVerify’s All Payer Advanced Eligibility Solution in Instant, Batch, or API Eligibility, in real-time with accuracy down to the service received.
Patient Estimator
Estimate patient financial responsibility powered by Eligibility results and your unique fee schedules for quick and easy cost estimates.
Healthcare APIs
The Industry service leader in Realtime Healthcare APIs for Eligibility, Claim Status, & DME Solutions.