Medical Insurance Eligibility Verification
Medical Patient Insurance Eligibility Verification
Medical Eligibility Verification Solution
Complete Patient Eligibility Verification
Eligibility Verification Solution
Insurance Eligibility Verification
Medicare Eligibility Check For Providers
Medicare Eligibility Verification
Insurance Verification
Insurance Verification software
Office Insurance Verification
Verify Insurance coverage online
Verify Insurance Online
Patient Eligibility Verification Software
Medicare verify insurance
how to verify insurance
Eligibility verification system
verify Medicaid eligibility
Verify Health Insurance
270/271
Verify Medical Insurance
All Payer Eligibility
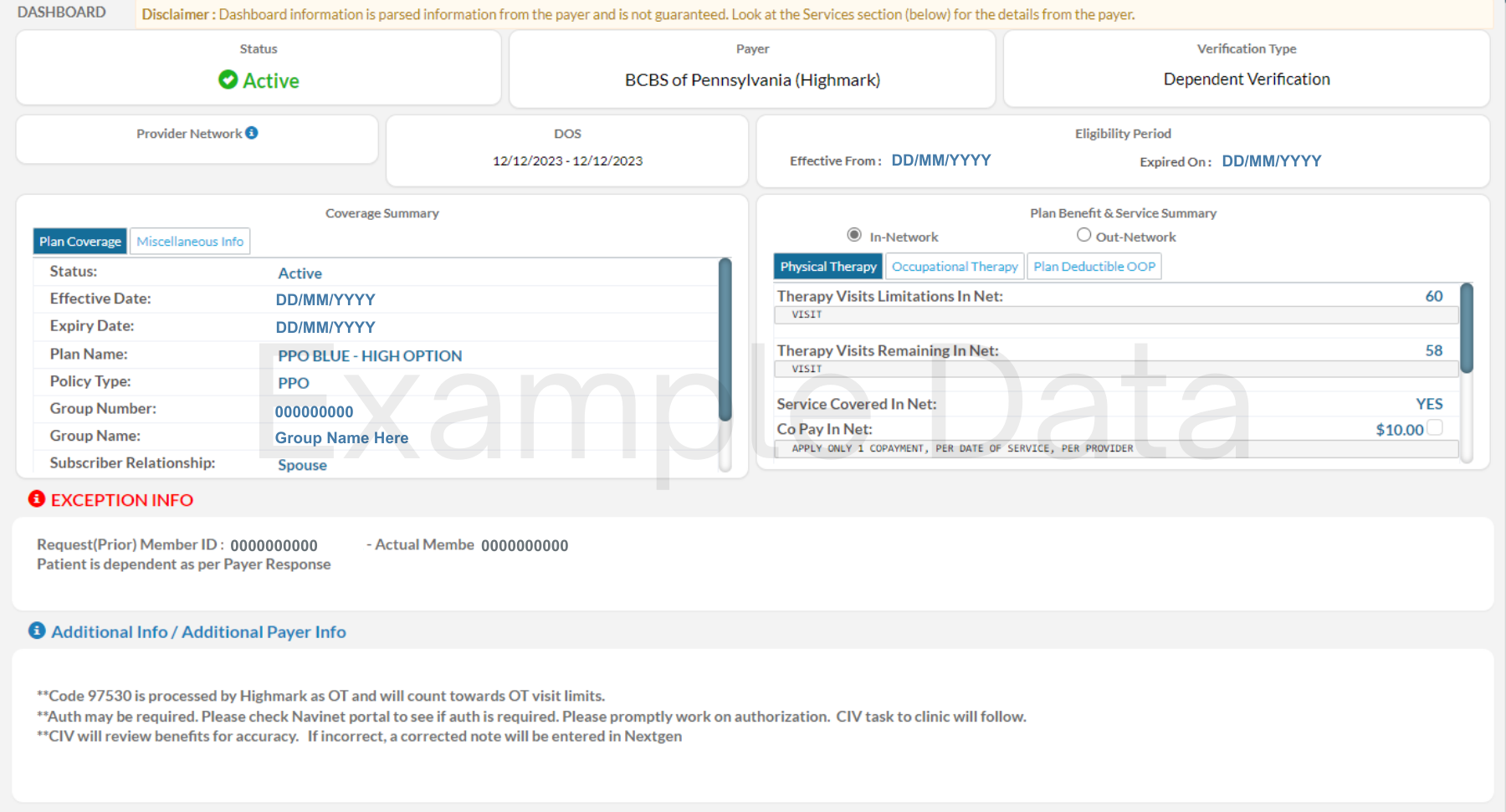
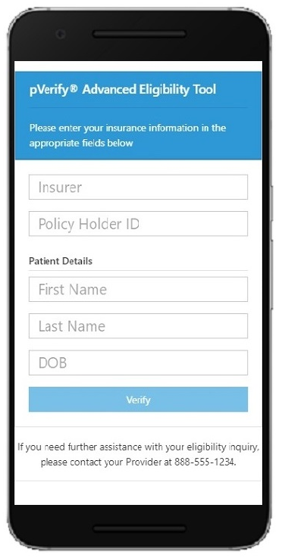
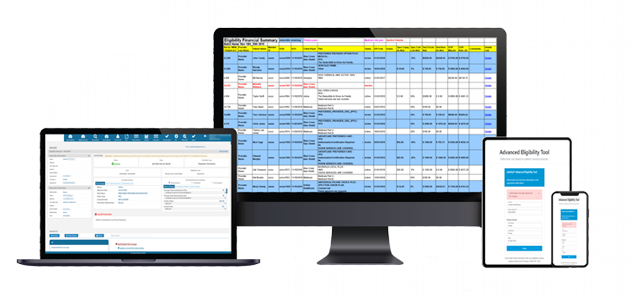
Build pVerify’s Advanced Eligibility Verification directly into your workflow
Going beyond Eligibility: Business Rules Engine
Business Rules is pVerify’s unique way of taking a client’s book of proprietary knowledge, the binder and post-it notes of information gathered over the years by experienced verification specialists and inserting that knowledge to be cycled through and reported on qualifying patient benefits. Based off of a Payer, Group Name/Number, Member ID, Plan Name/Number or Policy ID.
Add your verification specialist’s expert knowledge into pVerify’s Business Rule Engine, to be returned automatically on verified patient benefits.
With the largest Medical Insurance Eligibility Verification Payer List in the industry, pVerify is the only company to go beyond the traditional EDI payers to provide the eligibility benefits from the smaller and time-consuming non-EDI Payers. We provide details at a deeper level, with information separated and highlighted individually for easier review and understanding.
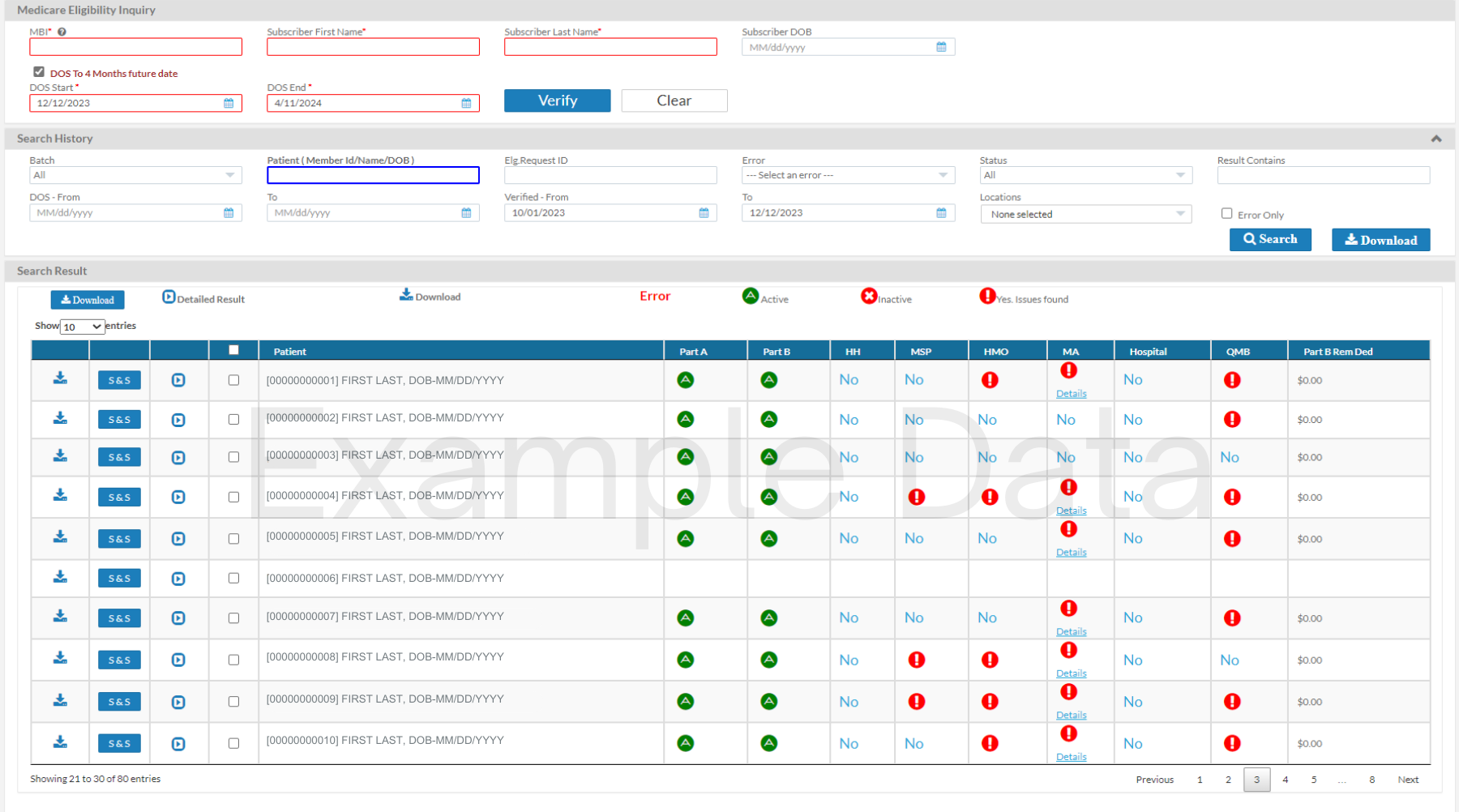
A leader in real-time Complete Patient Eligibility Verification, pVerify’s Advanced Eligibility provides more information than ever before for Medicare. Find what you need to see, from Episode Dates to HMO, PPO, and Plan Sponsor Details. Process Batches on your own with our Self-Batches Eligibility, view results on our Medicare Eligibility Summary Dashboard, run Estimations, collect Co-pays, and view Same or Similar and Inpatient Skilled Nursing Facility records with the click of a button.
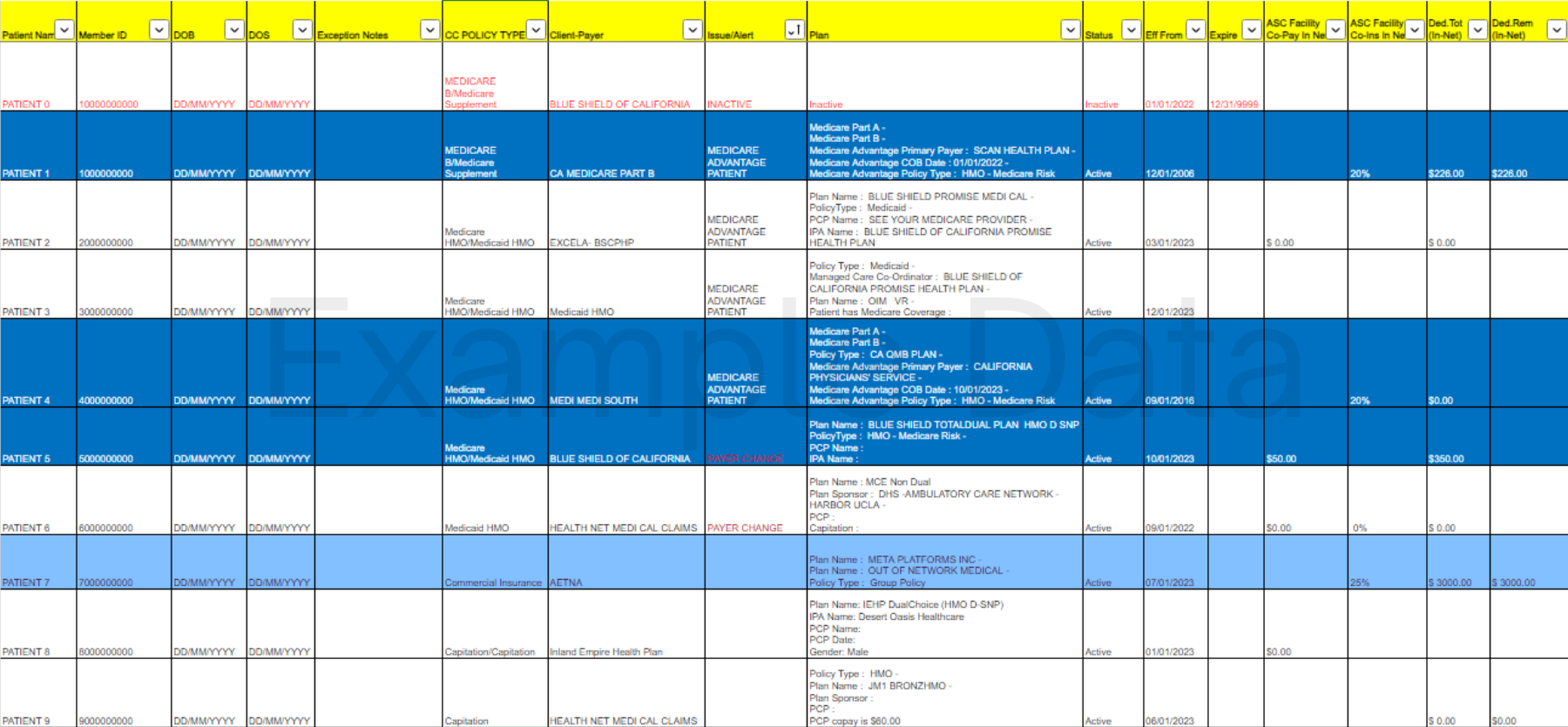
Medicaid patient verification is more complex on many levels. Be it the MCO, HMO, and Plan Sponsors, Medicaid simply supplies information differently than most other payers. Developed for this reason, pVerify First-Class Batch Reports can verify both levels, Medicaid and their MCO/HHO/Plan Sponsors, automatically and return benefits specific to what you are looking for. Additionally, Medicaid Insurance Discovery with Name/DOB and bi-monthly Active Status confirmation prevent future denials and allow for Retroactive Medicaid Claims.
The latest addition for the industry leader of Insurance Eligibility, pVerify has added Dental Payers to its Real-time Eligibility Verification Solutions. With requirements of a Dental NPI and Tax ID, pVerify users can now verify 150+ Dental payers in their secure Premium Portal. Dental is available via single patient verification, First-Class Batch Solution, and API Connection.
Update: As of September 2021 pVerify now offers real-time Vision Payer Verification in the Premium Portal and API Integration for VSP, Eyemed, March Vision, Premier, Davis, Spectera, and MORE!
Founded in 2006, pVerify’s first specialty of focus was Ophthalmology. Spending over a decade researching Vision benefits in our Medical Eligibility Verification Solution, pVerify added Non-EDI Vision Payers to their payer mix by enhancing their Non-EDI capabilities. Beyond the detailed vision benefits available with Advanced Eligibility, Material Coverage Details, PCP information, and Copay/Co-insurance details are available with the First-Class Batch Reports for VSP, Eyemed, Davis Vision and MORE!
Our unique blend of machine and human-enabled AI and ability to use business logic and manual means of obtaining information from traditional and more difficult payers. Beyond the detailed benefits available from EDI Payers, further details can be obtained through our Non-EDI Solutions, such as Material Coverage Details, PCP information, IPA Active Status, and benefits from payers not capable of EDI communication.
pVerify’s Insurance Discovery allows Hospitals and Providers to find a patient’s insurance coverage to collect potentially millions from insurance companies, allow prompt claim submission, increase patient payment collection, and drastically decrease Account Receivables.
Before providing service or afterward while prepping the claim, pVerify’s Insurance Discovery can detect up to 50% coverage for self-pays and incomplete patient files.
We have decided to begin using the services of a company called pVerify for our eligibility and verification of patients. Over the years I have dealt with a number of different companies that do batch and individual eligibility checks, and quite honestly the product pVerify has built is the best I have seen. Additionally, they allow me to customize my payers with business rules so the information that is returned to me for my team to work identifies authorization and referral requirements per the rules we build, as well as includes the laboratory information for where pathology needs to be sent. We are very pleased with their product.
Medical insurance eligibility verification
270/271
Insurance Verification
pVerify’s Unique Patient Eligibility Verification Solutions Features:
- Detailed Benefit Information
- Additional Features
- Specialty Specific Examples
- Start your Free Trial
- Verify - Estimate - Collect
pVerify provides Patient Insurance details at a deeper level, with information separated and highlighted individually for easier review and understanding
Traditional Details available with Eligibility Verifications
- View Plan Active Status with HMO/PPO Alert
- Detect HMO, PPO, MCO, IPA, and Plan Sponsor Names when verifying Secondary
- Capture Deductible & OOP allotted vs remaining
- Additional Payer Info (Plan Sponsor or CA IPAs)
- Standard Copay & Co-insurance details per Specialty.
- Exception Reporting – Identify spelling errors and typos in Name, DOB, and Member ID to send correct information on each claim.
Detailed Eligibility Verification Benefit Information
- Plan Name & Number, Policy Type, Group Name & Number
- Important Dates: Effective, Expired, Plan Began, Service Began.
- Learn if NPI is in Network (limited to participating payers)
- Payer Billing Address, ID, and/or Phone Number
- Co-pay, Co-insurance, Deductible applies to OOP details
- Individual and Family Deductible and OOP information
- Plan Group or Plan Network Tier information
pVerify aims to capture as much detail as possible through EDI, human-enabled AI, machine learning and manual effort. The availability of the above information varies and depends wholly on the payer.
Additional Features
- Home Health, Hospice, and SNF Dates for Medicare
- Multiple level verification for IPA Payers
- Issues (Inactive) and Exception Reports (Clean Claims) Included
- Eligibility information for Preventative Services such as Cardiovascular Disease Screening (CARD )(HCPCS|80061)
- Multiple Patient Batch Upload, Single Patient Verification, First Class Batch Processing, API Integrations, and EHR/PM Integrations available
- Primary Care Physician Details
Additional Solutions
- Patient Estimator
- Patient Payments
- Claims Status Check
- Same or Similar (Equipment)
- On-going Skilled Nursing (Billing NPI)
- Medicare CMN (Rentals)
pVerify aims to capture as much detail as possible through EDI, human-enabled AI, machine learning and manual effort. The availability of the above information varies and depends wholly on the payer.
Physical Therapy Examples
- If Prior Authorization is required
- Co-pays & Co-insurance details
- Physical Therapy visits included in benefits vs remaining
- Combined therapy details for visits allotted vs remaining
- Used amount of Therapy Cap for Medicare
- …and MORE!
Mental Health Examples
- If Prior Authorization is required
- Telemedicine and Virtual Visit Details
- Co-pay & Co-insurance details for multiple Behavioral Health Services including: Mental Health Facility & Provider, and Psychiatric, Psychotherapy & Substance Abuse – Inpatient/Outpatient
- Medicare Lifetime Days Reserve and Remaining
Ophthalmology Examples
- If Prior Authorization is required
- Co-pay & Co-insurance details
- If Routine is included in plan and available
- Surgical and ASCF Co-pay & Co-insurance
- Materials Information: Frames, Lenses, & Contacts
- Non-EDI Payer Verification: VSP, Eyemed, Davis Vision, etc
- Primary Care Provider Name
pVerify aims to capture as much detail as possible through EDI, human-enabled AI, machine learning and manual effort. The availability of the above information varies and depends wholly on the payer.
Verify Eligibility
- Verify a patient ahead of time or during their procedure with Instant, Batch, or API Eligibility, in real-time with accuracy down to the service received.
Estimate Patient Responsibility
- Estimate patient financial responsibility powered by Eligibility results and your unique fee schedules for quick and easy cost estimates.
Collect Payment
- Collect payment during appointment with hands-free options with QR code, card-on-file and customized card-on-file payment plans.
pVerify aims to capture as much detail as possible through EDI, human-enabled AI, machine learning and manual effort. The availability of the above information varies and depends wholly on the payer.
Connect to learn what pVerify’s Advanced Medical Insurance Verification Solution provides for your specialty!
Create your own combination of pVerify’s Solutions below
Schedule custom DEMO or Free Trial of pVerify’s Insurance Verification Solutions
Meet with a pVerify Representative to learn how to verify patient insurance, along with assessing your current verification work flow to determine the best combination of pVerify’s Medical Insurance Eligibility Verification Solutions for your needs.
More pVerify Solutions
Claim Status
pVerify’s Claim Status allows users to check the current status from the payer to discover the claim was accepted, or denied, and review the Status Codes to determine if action is required.
Patient Estimator
Estimate patient financial responsibility powered by Eligibility results and your unique fee schedules for quick and easy cost estimates.
Healthcare APIs
The Industry service leader in Realtime Healthcare APIs for Eligibility, Claim Status, & DME Solutions.
Healthcare APIs
The Industry service leader in Realtime Healthcare APIs for Eligibility, Claim Status, & DME Solutions.